ILINDPOS2500EliteG-
22
22,070
Health Alliance Medical Plans, Inc.
2023 POS 2500 Elite Gold
Member Responsibility
Member Benefits Participating (In-Network) Non-Participating (Out-of-Network
(OON))
Plan Year Deductible Medical Individual $2,500 $5,000
Embedded Family $5,000 $10,000
Pharmacy Individual Not Applicable Not Applicable
Family Not Applicable Not Applicable
Dental Per Member $120 Not Applicable
Plan Year Out-of-Pocket Maximum (OOPM)
Combined medical and pharmacy
expenses including deductible,
coinsurance & copayments.
Dental OOPM goes toward medical
OOPM
Contract Year Maximum Benefits
Ambulatory Patient Services
Medical/Pharmacy Individual $6,000 $17,500
Family $12,000 $35,000
Pediatric Dental Individual $350 Not Applicable
Family $700 Not Applicable
Cardiac Rehabilitation Services 36 OP sessions w/in 6 month of event combined in-net and OON
Outpatient Rehabilitation Services 60 visits per condition per plan year combined in-net and OON
Habilitative Services 60 visits per condition per plan year combined in-net and OON
Acupuncture Treatment 15 visits per plan year combined in-net and OON
Chiropractic Services 25 visits per plan year combined in-net and OON
Adult Vision Exam Once every 12 months.
Pediatric Vision Exam Once every 12 months combined in-net and OON
Pediatric Vision Materials Once every 12 months combined in-net and OON
Pediatric Dental Exam Once every 6 months combined in-net and OON
Pediatric Vision Therapy 12 visits for treatment of Convergence Insufficiency per plan year
Vision Exam *$20 per exam Not Covered
Virtual Visits *$0 visits 1-3, then $25 per visit Not Covered
Emergency Services
Primary Care Physician Office Visits *$25 per visit 50%
Specialty Care Physician Office Visits *$50 per visit 50%
Chiropractic Services *$50 per visit In Network Benefit Applies
Acupuncture *$25 per visit In Network Benefit Applies
Urgent Care Visits *$50 per visit In Network Benefit Applies
Allergy Treatment and Testing 15% 50%
Emergency Department Visits 15% In Network Benefit Applies
Emergency Ambulance Transportation 15% In Network Benefit Applies
Rehabilitative and Habilitative Services
Outpatient Rehabilitation Services (PT, OT, ST) 15% 50%
Inpatient Rehabilitation/Skilled Nursing Facility 15% 50%
Home Health 15% 50%
Diagnostic Services
Mental Health/Substance Use Treatment
MRI and CT Scans 15% 50%
Laboratory and X-rays 15% 50%
Outpatient Office Visits *$25 per visit 50%
Inpatient Services 15% 50%
Hospital Services
Outpatient Surgery/Procedures Facility Fee 15%
Outpatient Surgery/Procedures Physician/Surgeon Services 15%
Inpatient Hospitalization Facility Fees 15%
Inpatient Physician/Surgeon Fees 15%
50%
50%
50%
50%
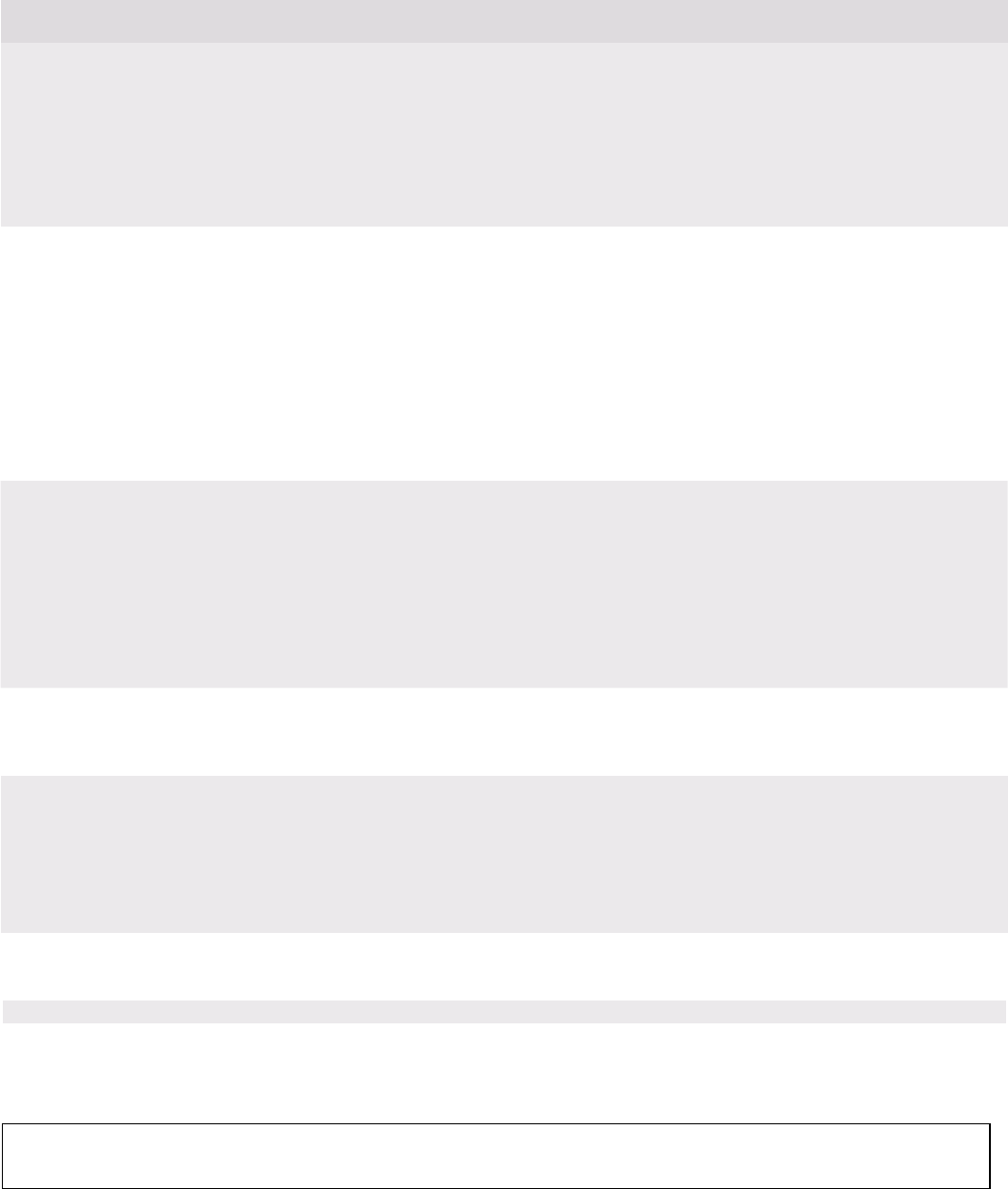
ILINDPOS2500EliteG-
22
22,070
Health Alliance Medical Plans, Inc.
Member Benefits
Participating (In-Network)
Non-Participating (Out-of-Network
(OON))
Prescription Drugs
30 day supply
Tier 1 - Preferred Generic
*$0
50%
Tier 2 - Non-Preferred Generic
*$10
50%
Tier 3 - Preferred Brand
*$40
50%
Tier 4 - Non-Preferred Brand
*$80
50%
Tier 5 - Preferred Specialty
*$150
50%
Tier 6 - Non-Preferred Specialty
*$250
50%
If you or your Physician requests a brand name drug when a generic drug exists, you pay the Preferred Brand or Non-Preferred Brand Deductible,
Copayment and/or Coinsurance, plus a 100% coinsurance for the difference in cost between the Brand name drug and the Generic drug. This price
difference is applied to your Deductible and Out-of-Pocket Maximum. In no instance will the total cost you are charged for the drug exceed the actual cost
of the drug.
Maternity
Minimum of 48 hours of inpatient care following a vaginal delivery and
minimum of 96 hours of inpatient care following a delivery by Cesarean
section.
Routine Prenatal Care
15%
50%
Maternity Inpatient
15%
50%
Newborn Care
15%
50%
Pediatric Services
(members up to the age of 19 years old)
Pediatric Dental Exam $0 per exam Not Covered
Preventive Dental Services *$0 per visit Not Covered
Minor Dental Restorative 50% Not Covered
Major Dental Services 50% Not Covered
Medically Necessary Orthodontia Services 50% Not Covered
Pediatric Vision Exam *$0 per exam 50%
Pediatric Vision Materials *$0 per item In Network Benefit Applies
Preventive and Wellness Services
Immunizations, adult & child annual physical exams, mammograms, PAP
smears, prostate exams & more. Age/frequency schedules apply.
Wellness Care *$0 50%
Other Services
Other services covered within your policy and not otherwise specified on
this summary or on the SBC.
Other Covered Services
15%
50%
Abortion Procedure Facility Fee
15%
50%
Abortion Procedure Physician Fee
15%
50%
Durable Medical Equipment
15%
50%
* Deductible does not apply
Embedded deductible definition - If two or more members have separate individual deductibles embedded within the family deductible. This gives
each member a chance to have his or her benefits start before the entire family meets the family deductible.
When using out of network providers, you also pay any charges in excess of the maximum allowable charge. Amounts over the maximum allowable
charge do not apply to the Out-of-Pocket Maximum.
This is a brief statement of Health Alliance
POS
benefits, exclusions and limitations which are subject to change. Please refer to the Health Alliance
POS Policy booklet for more detail about your health plan. This document is in conjunction with the Summary of Benefits and Coverage (SBC). You
can view your SBC online at www.healthalliance.org or request a copy by contacting the customer service number on the back of your ID card.
